The journal Nature Biotechnology recently published research results that appear to be a small step forward in improving islet cell transplantation. Islet cell transplantation is one of the four potential pathways to a Practical Cure, pending significant advances in cell supply and cell protection.
The key finding of the study is that a new procedure allows islet cells to be transplanted underneath the skin rather than into the liver. This improves both cell survival and monitoring. Many researchers have been seeking a solution to the problems associated with the current practice of transplanting islet cells into the liver, where a large portion of islet cells die.
The study was led by Dr. James Shapiro from the University of Alberta who is well known as a pioneer of islet cell transplantation and co-creator of the Edmonton Protocol.
Highlights:
- Results to date are from animal subjects, not humans. Shapiro expects to start human trials within 12 months.
- 91% of animal test subjects achieved insulin independence from islets transplanted under the skin.
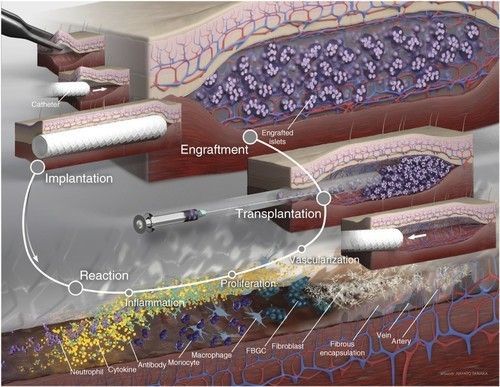
- The procedure: A thin plastic tube is temporarily inserted under the skin. The body’s natural response to foreign objects causes new blood vessels to grow in the area. After the tube is removed, the new blood vessels supply nutrients necessary for engrafted islet cells or stem cells to survive.
- This research on its own is not a Practical Cure, but may be a component of one. To be a Practical Cure, islet cell transplantation will require advances in multiple research components, including:
- Site selection: creating a site in the body where implanted islet cells can thrive.
- Islet cell supply: finding an alternative source of islet cells than cadavers, which have very limited availability.
- Targeted immunosuppression: refining immune-suppressing drugs to have fewer side effects and effectively control only limited portions of the immune system.
