The definition of a Practical Cure was developed based on the wishes and desires of people who are currently living with type 1 diabetes. It is defined as any solution which minimizes the disruptive aspects of T1D and delivers a near-normal quality of life. Over the past seven years, a point of view to prioritize the pursuit of a Practical Cure over all other types of research has been voiced time and again by the T1D community.
A Practical Cure is Outcome Focused
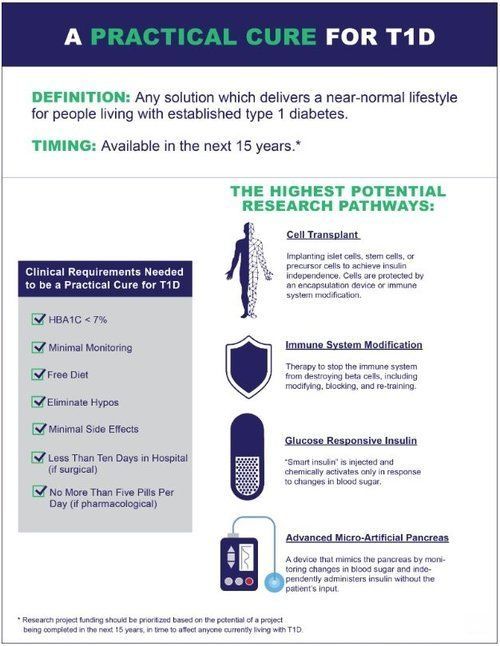
The opening chart shows the various outcome criteria that a Practical Cure must meet, including sleeping worry-free, no dietary restrictions, minimal monitoring, insignificant side effects, elimination of hypos, and HbA1C readings under seven percent. Any research approach, pathway, or philosophy that can deliver these outcome objectives is valued and merits pursuit.
A Practical Cure is Time Bound
One critical aspect of a Practical Cure solution is that it must be available within the next 15 years. The rationale for 15 years— which reaches further into the future than most of us actively think about— is rooted in the amount of time a clinical trial requires to advance through the FDA approval process. On average, a successful project takes 10-15 years to progress through all of the FDA clinical trial testing phases.
A 15-year goal means that any project that is currently in human trials, or about to start human trials, has a reasonable chance of advancing through clinical trials and receiving approval for public use and commercialization. Projects that have not advanced to human testing and are currently testing in mice are unlikely to make it to market in the next 15 years.
There are two essential benefits to having a time goal. The first and most important benefit is that a time goal stresses the importance of delivering a solution in time to transform the lives of everyone living with the disease. A time goal puts the emphasis on helping people who are currently living with the disease as opposed to focusing on a cure for future generations.
The second important benefit of a time goal is that it provides a structure for prioritizing projects. The JDCA believes that projects that have already advanced into human trials should be given priority, fully funded, and wholly resourced so they can move through human trials to conclusive results as quickly as possible. In our view, projects that do not have a chance of being available in the next 15 years should receive lower priority in terms of research funding.
The Pathways
- Cell Transplant with Autoimmune Protection involves implanting islet cells, stem cells, or precursor cells into a person with type 1 diabetes to achieve insulin independence. There are currently three active projects in human trials.
- Immune System Modification with Sustainable Cell Supply stops the body’s immune system from attacking insulin-producing beta cells using drugs or stem cell therapy. Currently, human trials are testing the utility of regenerating beta cells alongside immunotherapy in type 1 diabetics with the goal of producing sufficient amounts of insulin. If regeneration proves ineffective, blocking the autoimmune attack would need to be combined with islet cell transplantation. There are currently eight active projects in human trials.
- Glucose-Responsive Insulin, aka “smart insulin,” is chemically activated in response to changes in blood glucose. Once injected, smart insulin remains inactive until blood glucose rises above normal levels. At that point, the chemical component activates the insulin, and once blood glucose returns to normal, the insulin action ceases, avoiding low blood sugar. To qualify as a Practical Cure, smart insulin would have to last long enough to eliminate the need for multiple daily injections. There are currently no active projects in human trials.
- An Advanced Micro-Artificial Pancreas is under development at several commercial and academic centers. However, no current devices are small enough to be considered a Practical Cure. The JDCA recently completed a survey asking the T1D community to identify the requirements an artificial pancreas must meet to qualify as a Practical Cure. 88 percent of respondents said an AP device would be a Practical Cure if "it is small enough that you could generally forget that you are wearing it." Although no current devices are small enough to meet the Practical Cure threshold as defined by people living with T1D, technology has a way of evolving quickly. Consequently, the JDCA is hopeful there will be size and reliability breakthroughs in the near future.
